What is pharmacogenomics?
… and how can clinicians take advantage of advances in genomics to better predict how their patient will respond to medication?
Pharmacogenomics is the study of how a patient’s genome can influence how they respond to medicines. Variants in an individual’s genome can increase the functioning of medicines or make them ineffective. They can also help predict which patients will suffer from side-effects – from the merely unpleasant to potentially life-threatening. Pharmacogenomics can help clinicians decide what drugs to give a patient, and at what dosage.
Why is this important? It’s thought that drug interventions are effective in just 30%-60% of patients because of the difference in how individuals respond to medication. One in 15 UK hospital admissions is linked to adverse drug reactions, costing the NHS more than £600m each year.
So, with good reason, pharmacogenomics is one of the three main goals of the NHS genomic revolution, along with improving outcomes in cancer and rare diseases. By using genomic information to get more patients onto the right treatment quickly, the NHS hopes the cost of genomic testing will be outweighed significantly by reducing wasted prescriptions, minimising unnecessary hospital admissions and saving clinicians’ time.
Let’s take a look at two key ways in which pharmacogenomics can improve healthcare.
Avoiding adverse reactions
A drug may have a low risk of side-effects in the general population, but a high risk in a group who possess a certain allele (a variation in their genome). An example of this is abacavir, an antiviral medicine that is used as part of combination therapies for HIV. Abacavir is well tolerated by most patients, but a small number (around 5%) will have a hypersensitivity reaction to it, which can be severe and is occasionally fatal.
The risk of a hypersensitivity reaction is much higher in patients who have a particular gene variant called HLA-B*5701, and NICE guidelines state that patients should be tested for this prior to commencing treatment. This test has been available for over a decade and researchers have found that it has a major impact on the frequency of hypersensitivity reactions.
Deciding dosage
A patient might metabolise a drug faster than normal – so it is removed more quickly from the body and does not have sufficient effect. Or a person may metabolise a drug slowly, so it builds up in their system and can become toxic.
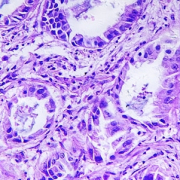
An example of this is the class of drugs known as thiopurines, which have applications in chemotherapy, and also as immunosuppression in autoimmune diseases. When given in excessive doses they can cause dangerous side-effects. As well as the dangers that these pose, they can cause the need to pause therapy, which could reduce the likelihood of the chemotherapy being successful.
An enzyme called thiopurine methyltransferase (TPMT) is involved in metabolising thiopurines. Around 3 in 1,000 people have no working copy of the TMTP gene, and closer to 10% have a version of the gene that is less active than the rest of the population’s. In these individuals, a standard course of treatment could cause them to become extremely ill.
NICE does not currently recommend a gene test, but advises clinicians to “consider measuring TPMT activity before starting azathioprine, mercaptopurine, or tioguanine therapy. Patients with absent TPMT activity should not receive thiopurine drugs; those with reduced TPMT activity may be treated under specialist supervision.”
In time, as whole genome sequencing becomes available to patients with hard-to-treat cancers and severely ill children, the clinicians treating leukaemia patients will hopefully have this information at their fingertips.
Pharmacogenetics or pharmacogenomics?
Often used interchangeably, the term pharmacogenetics refers to the impact of a single gene on the interactions between one specific medicine (or group of medicines) and the body, while pharmacogenomics looks at how all the regions of the genome (both coding and non-coding) can regulate drug responses.
For example, the abacavir test is for a single gene – this can have the advantage that a result can be generated more quickly than a whole genome sequence and may require less complex interpretation. For patients who are likely to need several tests, however, a whole genome sequence may offer better value than multiple single tests, especially if costs and processing times continue to fall.
As the national NHS Genomic Medicine Service is rolled out over the next year, we will update on any new developments in pharmacogenomics testing that emerge following the current test directories for cancer and rare diseases.
–