More than skin deep: genomics and dermatology
Improved understanding of the genetic basis of skin conditions is enabling better treatment for patients
Dermatology is just one of the medical specialties benefiting from genomics. Uncovering the pathology of disease at a molecular level allows specialists to offer more effective diagnosis and management, and opens up the possibility for new treatments to be developed.
Diagnosing rare diseases
One in 17 people in the UK is affected by a rare disease, so, despite each individual disorder being rare, together rare diseases make up a proportion of the clinical caseload in most specialities. Dermatologists are aware of a range of genetic skin conditions caused by rare mutations, termed ‘genodermatoses’. These include forms of ichthyosis, Xeroderma pigmentosum, palmoplantar keratoderma and pachyonychia congenita. Whilst many such conditions have no cure, early diagnosis and careful clinical management to improve quality of life and prevent complications is important – but not always easy.
Genome sequencing technologies could have a significant impact on diagnosis of epidermolysis bullosa (EB), a group of rare inherited skin disorders that cause the skin to become very fragile. The different subtypes of EB vary in prognosis and therefore specific diagnosis of a subtype is important for patient management. Currently, diagnosing EB sub-types is a step by step process; methodologies include skin biopsy for immunohistochemistry and transmission electron microscopy, in addition to traditional, targeted DNA sequencing of candidate genes. However, high-throughput genome sequencing technology makes it possible to sequence multiple genes simultaneously, enabling faster diagnoses and access to more appropriate treatments for individuals.
Helping to understand common complex diseases
Investigations of rare genodermatoses can also improve understanding of related common complex diseases – those caused by a combination of environmental factors and underlying genetic susceptibility.
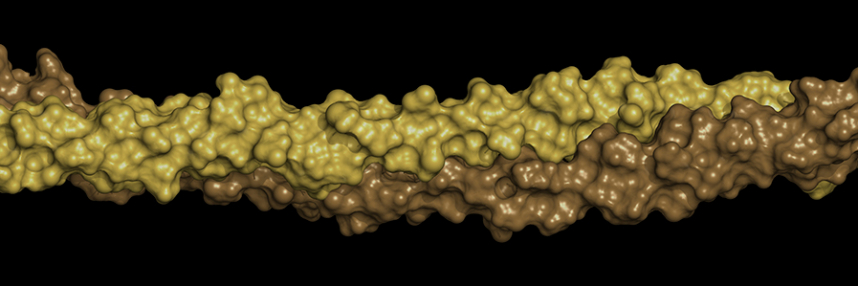
For example, studies have linked mutations in the gene for the filaggrin (FLG) protein with the inherited dry skin condition ichthyosis vulgaris (IV). FLG is produced in the epidermis, and when ‘faulty’ creates a defective skin barrier. Many patients with IV also suffer from the common inflammatory skin disease atopic dermatitis (eczema), and this led scientists to carry out subsequent studies, which showed that genetic mutations are a significant risk factor for atopic dermatitis, as well as for the associated conditions atopic asthma, hay fever and peanut allergy.
Recently, the largest ever genome-wide association study of atopic dermatitis (AD) shed new light on its underlying disease mechanisms. The study found 10 new genomic regions with apparent ties to AD, bringing the total known for the disease to 31. The new regions include genes with roles in the regulation of innate host defences and immune T-cell function, underlining the important role the immune system plays in the development and progression of AD. In addition to current therapeutic approaches to maintain the skin barrier in AD, the findings suggest that treatments that target the immune system could be beneficial.
Deciding when to use genomic tests, and how to interpret their results, will become integral to medical practice in many areas, and health professionals across the health service will need to become more aware of their benefits in order to improve treatment for patients with a wide variety of conditions.
As well as Heath Education England’s MSc in Genomic Medicine and continuing personal and professional development modules (CPPD), work is also afoot to develop genomics knowledge and practice within individual specialties, including dermatology.
–