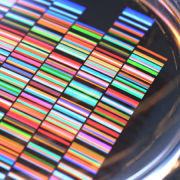
Whole genome sequencing drives progress in cancer
A new study into metastatic cancers highlights the significant potential for WGS in deepening understanding and improving treatment options
In the largest study of its kind, researchers in the Netherlands have used whole genome sequencing (WGS) to investigate what drives metastatic cancers, in turn kickstarting further research into treatment options for patients.
Metastatic cancers occur when cancer cells spread from the site of origin to other parts of the body. Around 90% of cancer deaths are due to metastasis, and researchers are working to understand more about these tumours – which are often resistant to standard therapies.
Why whole genome sequencing?
The researchers in the Netherlands used whole genome sequencing on 2,520 tumour samples from 2,399 individuals with various metastatic cancers. They also sequenced DNA from each patient’s healthy blood cells for comparison.
By using whole genome sequencing, which provides information on all of the tumour DNA, the researchers were able to identify over 70 million changes in the tumour genomes, from localised changes such as point mutations, small insertions and deletions to large structural variations, including translocations of DNA between chromosomal regions.
Structural variations are often missed when only portions of the genome are sequenced – for example with whole exome sequencing, which is widely used in clinical studies because it is less costly than WGS – but their discovery may have important implications.
Important discoveries
The researchers’ analyses confirmed the results of previous studies that failed to identify specific mutations ubiquitous among metastatic, but absent in primary, tumours. This supports the hypothesis that metastasis-specific mutations are not the main trigger for cancer to spread.
Some types of mutation were more common in metastatic tumours, but these varied across different cancer types: for example, in metastases from lung cancer or melanoma primaries, point mutations were more common.
In more than half of the tumour samples, whole genome duplications (WGD) were present, and this figure rose to 80% in esophageal tumours. This compares to a reported rate of 30% in primary tumours. WGD are associated with resistance to chemotherapy drugs.
Treatment implications
‘Actionable variants’ were found in the tumour genomes of 62% of the patients in the study (meaning their tumours contained biomarkers which indicated that the patients could benefit from particular treatments). Half of the variants discovered matched with treatments currently in clinical trials; the rest could respond to cancer drugs that are already approved, but in many cases the application would be considered ‘off label’ as the drug is only approved for a different type of cancer.
A clinical study programme allowing patients to receive off-label medications has been set up by the Hartwig Medical Foundation in the Netherlands. Patients’ tumour and blood samples are collected in hospitals and sent for DNA analysis.
“The cohort is still expanding,” the authors note, “with data from 4,000 patients already available, and includes data that go beyond the basic clinical and genomic data analysed in this paper such as post-biopsy treatments and responses, and previous treatment information.”
The first results from the trial have already been published, and so far 34% of patients who received an off-label treatment benefitted.
The researchers have made their data from the study open access so that other scientists and clinicians can use it. They hope it will “provide a valuable complementary resource to whole-genome sequence-based data of primary tumours … in advancing fundamental and translational research.”
–