The role of genomics in assisted reproduction
As medical understanding of genetic variation increases, genomic technologies are providing hope for assisted reproduction
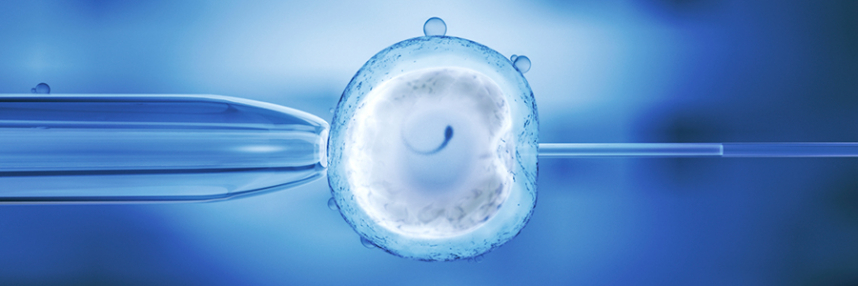
Last week saw the 37th birthday of Louise Brown, the world’s first ‘test tube baby’. Conceived by the in vitro fertilisation (IVF) technique pioneered by Patrick Steptoe and Robert Edwards, Louise was born in 1978 and the media have closely followed her every milestone – including when Edwards was awarded a Nobel Prize for Medicine in 2010 for his work in assisted reproduction.
Today, the total number of babies born as a result of IVF is approaching six million worldwide, and genomics is playing an increasingly important role. Genome sequencing technology now enables health practitioners to screen embryos for abnormalities before implantation, and this relatively modern development is expected to improve the efficacy of assisted reproduction.
Pre-implantation genetic diagnosis
Genetic screening was first applied in the context of IVF in the mid-eighties, with the introduction of pre-implantation genetic diagnosis (PGD). This technique was developed to assist couples at risk of having a child with a serious, heritable disease, following previously affected pregnancies or a family history of genetic or chromosomal disorders. The process involves IVF embryos being analysed genetically, with only unaffected embryos selected for implantation. Before PGD, couples deemed to be at risk had had to wait for invasive testing during established pregnancies, risking an increased chance of miscarriage.
Improving IVF through genomic screening
More recently, the genetic analysis of embryos prior to implantation has also been used to help apparently healthy couples with no family history of genetic disease. Pre-implantation genetic screening (PGS) is a technique used to assess IVF and ICSI embryos for common abnormalities, notably for aneuploidy, an abnormal number of chromosomes responsible for various diseases.
The failure rate of IVF is relatively high, especially among women over the age of 35. The primary reason for this is that chromosomal abnormalities in a woman’s egg cells become increasingly common as she ages, and most embryos with such abnormalities fail to implant, or miscarry (this is true for natural as well as assisted conception). Genetic analysis can provide a dilemma for expectant parents: whether to terminate a wanted pregnancy or raise children affected or at risk of being affected by a potentially severe and sometimes fatal disability. But identifying the most genetically healthy embryos for implantation increases both the chance of a healthy pregnancy and the birth of a healthy child. Rapid screening of the egg cells themselves for selection prior to fertilisation is also possible.
Going for (genomic) gold?
As our capacity for genomic analysis and diagnosis has become rapidly more advanced, so too has its use in assisted reproduction. There was a time when genomic analysis was limited to detecting aneuploidy, but the advent of comparative genomic hybridisation has made it possible to spot smaller chromosomal defects as well. In 2013, Connor Levy became the first baby born following the use of advanced ‘next-generation’ DNA sequencing techniques to assess the genetic health of IVF embryos; and in 2015 it was revealed that whole genome sequencing of embryos may soon be offered routinely as part of IVF treatment. Such testing could reveal gene variations that may cause disease, but, as we have a limited understanding of the impact of innumerable variations, the great conundrum will come when determining which (if any) have significant medical implications.
–