Non-coding RNA: another piece in the atherosclerosis puzzle
Why do some conditions affect us more as we age? A recent study looked at one in particular, atherosclerosis, and found that non-coding RNA may hold the answers
Recent research by Brigham and Women’s Hospital in Boston, US, and published in Science Translational Medicine, has revealed a link between a specific long non-coding RNA (lncRNA), SNHG12, and an increased risk of becoming affected by atherosclerosis as we get older because of how it interacts with other molecules in the genome.
The role of non-coding RNA
Only 2% of the human genome encodes proteins. The other 98%, referred to as non-coding, is not fully understood, but is believed to be responsible for many regulatory functions, including the activation, suppression and stabilisation of other molecules.
Within this part of the genome are instructions for long non-coding RNAs (LncRNAs), a type of RNA that is not translated into a protein, and these have been studied to see if they hold the answers to longstanding questions about conditions like atherosclerosis.
What is atherosclerosis?
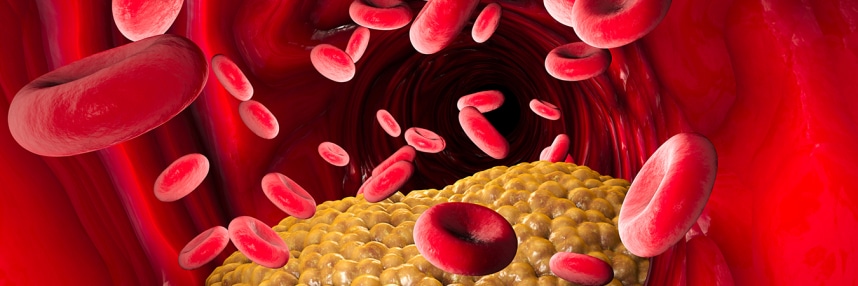
Atherosclerosis is a condition where fatty substances, called plaques, build up in the body’s arteries, causing them to narrow and harden. This can restrict blood flow and, in turn, cause a range of serious health problems, including stroke, heart attacks and kidney disease.
Risk factors for atherosclerosis include high cholesterol and high blood pressure, as well as smoking, obesity, insulin resistance and a sedentary lifestyle. If the disease is identified, treatment can reduce the risk of arteries becoming blocked through medications that lower blood pressure, cholesterol or the blood’s ability to form clots.
Atherosclerosis generally does not have symptoms at first, and affected people may not be aware of it until it causes more serious problems. Further, the likelihood of being affected by the condition is known to increase with age, though the genetic cause of this correlation has never been clear.
Clues in the transcriptome
In the study, which aimed to investigate why a diagnosis of atherosclerosis becomes more likely as we age, the researchers began their testing on mice, analysing the transcriptome (all the RNAs in a cell) of cells that line the blood vessels.
The transcriptome, unlike the genome, is dynamic; as the cell responds to different conditions, different parts of the genome are expressed, and this generates different RNAs. Some of these will be translated into proteins; others will have regulatory functions, like LncRNAs. The transcriptome offers a snapshot of the cell at a particular time, whereas the genome remains mostly the same throughout life.
The researchers compared transcriptomes from samples where the disease was progressing or improving, and looked for RNAs whose expression was very different in the two states. One that showed a marked difference was an LncRNA called SNHG12, which does not code for a protein.
“We have identified a new actor in controlling aging in the vessel wall and, surprisingly, it’s not a traditional gene or protein. It’s part of the non-coding genome. That was unexpected.” said Brigham and Women’s cardiovascular medicine specialist Dr Mark Feinberg, who led the research.
The impact of SNHG12
LncRNAs are present in the cells of all living organisms, and we know that the gene SNHG12 is present in humans, as well as mice and other mammals.
The researchers discovered that mice with an impaired ability to produce the gene product SNHG12 developed much more severe atherosclerosis, and mice given injections of SNHG12 had reduced disease progression.
They compared the findings to samples from humans and pigs, and found that, in both cases, SNHG12 levels were reduced in specimens with atherosclerosis.
Effects on DNA damage repair
The team followed up by looking at other molecules that SNHG12 is known to interact with. They discovered that it is associated with a DNA-dependent protein kinase (DNA-PK), which is important in regulating cell response to DNA damage.
When SNHG12 is reduced, DNA-PK does not bind with other molecules that initiate DNA damage repair. The result is that the cells senesce, and the vessel walls become permeable to LDL cholesterol, allowing plaques to form.
Dr Feinberg added: “We know a lot about the importance of cholesterol and inflammation in heart disease, but this is a new, additional pathway. We need to think carefully about how it might impact the development of therapeutics for cardiovascular disease.”
–