Tuberculosis: new approaches to an old disease
Recent developments show how genetic insight can help to combat the ‘forgotten plague’ that continues to kill
Tuberculosis (TB), once such a deadly foe that it has been referred to as ‘Captain of all these men of death’, has been less of a problem in the UK in the last fifty years due to a combination of factors – better housing and living conditions and, of course, effective antibiotics. Even so, TB never really went away, remaining a major public health issue around much of the world and in recent years, the threat it poses to the UK population has been increasing.
Hard to treat – a modern and deadly problem
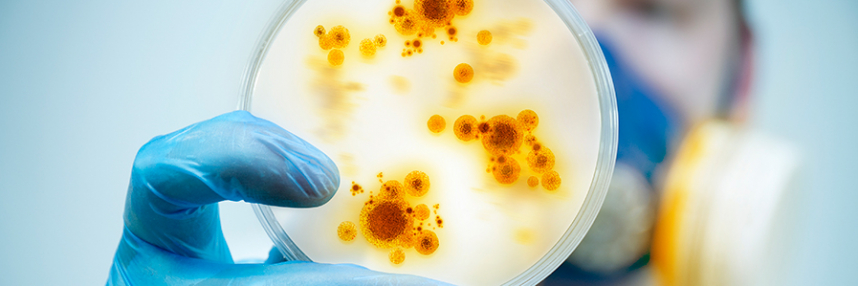
The disease is caused by the relatively slow growing Mycobacterium tuberculosis, and has never been easy to cure, requiring treatment over many months, sometimes years, to eliminate the infection. Poor compliance with drug treatment schedules has helped to drive the emergence of mycobacterial strains resistant to traditional drugs, which has gradually progressed to the development first of multi-drug resistant (MDR), then extensively drug resistant (XDR) strains, and finally even to effectively untreatable varieties. Since there is also no vaccine available, the spread of drug resistance means that TB is rapidly regaining prominence among threats to public health.
The quest for new forms of antimicrobial drugs and the scrupulous stewardship of remaining antibiotics has finally been recognised as a national (and global) priority, but meanwhile, people are still contracting and passing on TB, and the risk that existing drugs may be ineffective to treat it is rising.
Harnessing human immunity to target TB
Some researchers have taken a radically different approach in their quest for new treatments for this ancient disease. Rather than trying to design drugs to combat the mycobacteria, they have developed treatments to stimulate the body’s own defence systems against the infection – a technique dubbed host-directed immunotherapy. They found that using interleukin-1, which regulates the body’s immune responses, could effectively ‘dampen down’ the immune response mechanisms to M.tuberculosis infection that are associated with increased disease severity, by stimulating production of a molecule called prostaglandin (PGE2). Host-directed immunotherapy, using PGE2 and an asthma drug called Zileuton, was able to prevent death in TB-infected mice.
More recent research has shown that genetic changes in human lung cells which enhance interleukin-1 production can also help protect against TB. Also a study of genetic differences between humans that affect their susceptibility to TB infection has highlighted common variations in the gene for a protein called Mal that affect how it responds to immune system mediator interferon-gamma. It is hoped that testing for these genetic variants could help personalise TB treatments by suggesting whether or not giving the patient interferon would help them fight the infection.
A multi-pronged attack?
Other researchers are using genomics to identify potential targets for new TB drugs, and to improve existing ones. Taken together, genetic insights such as these could help in the quest for effective new treatments against TB. In the future, a combination of therapies directed against the specific strain of M. tuberculosis (characterised by genomic analysis) and those that stimulate the specific genetically determined nature of the patient’s own immune system could provide a vital therapeutic solution.
–