Healthy baby hope for those affected by mitochondrial disease
Seven women with a high chance of passing on genetic variants that cause mitochondrial disease have given birth to eight children with no sign of the condition, following pioneering IVF treatment
Researchers have announced a significant breakthrough in reproductive and genomic medicine after the delivery of eight healthy infants conceived through mitochondrial donation treatment.
The team, based at Newcastle University and The Newcastle upon Tyne Hospitals NHS Foundation Trust, has developed a new technique using donor eggs to reduce the chance of children inheriting mitochondrial disease from their mother’s DNA. The resulting babies – four girls and four boys, including a set of identical twins – are all developing normally, giving hope to other potential parents.
What is mitochondrial disease?
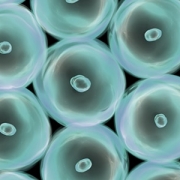
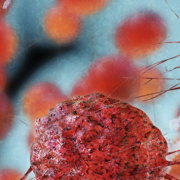
Mitochondrial disease is an inherited condition caused by variants in mitochondrial DNA (mtDNA), which are passed from mother to child. Mitochondria are the parts of the body’s cells that produce energy. Major organs such as the brain and heart, along with muscles, can be badly affected if mitochondria do not work properly. In some cases, the condition can be fatal.
As there is no cure for mitochondrial disease, mitochondrial donation offers affected families a chance to have genetically related children without passing on the disease.
The transfer process
The Newcastle team’s new treatment involves a technique called pronuclear transfer. Nuclear DNA from a fertilised egg of a woman with variants linked to mitochondrial disease is transferred into a donor egg with healthy mitochondria, from which the donor’s nucleus has been removed. This results in an embryo with nuclear DNA from the parents and healthy mitochondria from the donor, reducing the chance of mitochondrial disease transmission. Around 99.9% of the child’s DNA is inherited from the mother and father, with the remaining 0.01% coming from the donated mitochondria.
Although three of the eight babies from the Newcastle programme had health issues in their early months, the team say they do not believe these were linked to mitochondrial donation, or to the mother’s mitochondrial DNA. One of the problems resolved itself without treatment, with a second responding quickly to antibiotics. The third, say the team, is being successfully treated.
Impact on families
For families affected by mitochondrial disease, the possibility of having healthy, genetically related children is life changing.
Liz Curtis started The Lily Foundation after the loss of her daughter. She describes what the new treatment means for families affected by mitochondrial disease. “We fought long and hard for this change so that families could have choices,” she says. “After years of waiting, we now know that eight babies have been born using this technique, all showing no signs of (mitochondrial disease). For many affected families, it’s the first real hope of breaking the cycle of this inherited condition.”
For the mother of one baby girl born following mitochondrial donation, that hope has become reality. She says: “As parents, all we ever wanted was to give our child a healthy start in life. Mitochondrial donation IVF made that possible. After years of uncertainty, this treatment gave us hope — and then it gave us our baby. We look at them now, full of life and possibility, and we’re overwhelmed with gratitude. Science gave us a chance.”
Carryover potential
One of the challenges with mitochondrial donation is the potential for carryover, in which a small amount of unhealthy mitochondria is transferred during the process. There is also the concern of reversion, in which these small amounts could multiply during later development.
In the eight healthy babies, the Newcastle team found no significant carryover issues. In five of the children, levels of unhealthy mitochondria at birth were undetectable. In the other three, the highest levels were still well below the clinical threshold for symptoms. In one child, unhealthy mitochondria levels decreased over time and were undetectable by 18 months.
Continued monitoring of the children is part of a comprehensive follow-up process, allowing early detection of any emerging issues.
Ongoing research
Despite these positive outcomes, senior research team member Professor Mary Herbert acknowledges that there is still more to do. “The findings give grounds for optimism,” she said. “However, research to better understand the limitations of mitochondrial donation technologies will be essential to further improve treatment outcomes.
“Mitochondrial donation technologies are currently regarded as risk-reduction treatments, owing to carryover of maternal mitochondrial DNA during the mitochondrial donation procedure. Our ongoing research seeks to bridge the gap between risk reduction and prevention of mitochondrial DNA disease by addressing this problem.”
New hope for affected families
Mitochondrial donation reduces the chance of inherited mitochondrial disease rather than eliminating it entirely. The aim is to further improve outcomes through ongoing research.
The birth of eight healthy children through mitochondrial donation in the UK is a major scientific, clinical, and ethical achievement. It demonstrates the power of medical innovation when guided by rigorous research, regulatory oversight, and advocacy. The success of the Newcastle team has opened a new path for families affected by mitochondrial disease, offering real hope for future generations.
Read our two-part blog series to find out more about mitochondrial disease and developing treatments.