In this teaching scenario, Graham talks about the role family history played in his diagnosis and how he has changed his lifestyle
A male who was in good health and who had a heart attack at the age of 67 discusses how a chance conversation with another patient prompted him to think ‘family history’. Graham also explains how his lifestyle has changed and the impact for his other family members following his diagnosis.
Read Graham’s story below and use the teaching moments and discussion points to design your teaching session.
AT-A-GLANCE
Clinical focus: Cardiology, common conditions
Nursing activities: Communication, management, family care, referral, identification, treatment, prevention
NMC platform and outcomes: 1 (1.9, 1.13, 1.14, 1.18); 2 (2.4, 2.5, 2.8, 2.10); 3 (.2, 3.3, 3.5, 3.6, 3.11, 3.12, 3.15, 3.16); 4 (4.2, 4.3, 4.5, 4.17); 5 (5.4); 7 (7.1, 7.8)
Graham’s story
Identification
1 It all started at about 6pm on 7 June 2002. There I was with my family and friends when I felt tired and unwell and went upstairs to bed. My wife was about to call the doctor when I said to her “call an ambulance”. Immediately afterwards, I had the most terrible pain across my chest and I couldn’t breathe. I had a heart attack. Looking back, there were some signs of shortage of breath several weeks before which I had ignored.
2 The paramedics arrived shortly afterwards, gave me oxygen and I was off to hospital for six days. I was given a range of tests, but I did not see a consultant cardiologist. Twice, I complained about discomfort in my chest in hospital, but this was attributed to indigestion. When in hospital, a conversation with two other heart attack patients really made me think: our fathers all had heart attacks and, guess what, at exactly the same age that each of us had heart attacks. In my case, I was 67 years old at the time and my father died when he was 67. I will never forget that conversation! Next day, I was discharged from hospital with an appointment to see a cardiologist six weeks later.
3 Next day at home, I had chest pains when inactive and I was sure I had unstable angina. My excellent GP referred me to a cardiologist. I had an angiogram and, two days later, a heart bypass.
4 After having taken my health for granted until then, I thought I had better find out a bit more about my family and heart problems, especially in view of the conversation I had with the other patients in hospital. In general, I found out that females live about 20 years longer than the males in my family. My mother died at 89 and her sisters mostly in their eighties and nineties; my uncles died in their fifties and sixties, mainly from heart problems. Some of the surviving females suffered from stable angina, but my uncles died from heart attacks.
Management
5 I have two sons and eight grandchildren. What do I do? I can’t change their genetics. Fortunately, I attended a cardiac rehabilitation course through the NHS and learned a bit about lifestyles. I realised that cardiac risk factors were worth studying. I also studied British Heart Foundation booklets which contain some excellent information and I strongly recommend them.
6 My father smoked and had an unhealthy diet, but exercised a reasonable amount. He was a relaxed character and did not take alcohol. I do not smoke, had a reasonable diet and exercise a lot. I have my mother’s temperament of wanting to get things done and I drink moderately, about 10 units per week. After studying risk factors, I decided to change my diet by reducing salt intake and levels of saturated fats.
7 I take 75 milligrams of aspirin and one beta blocker each morning, and a simvastatin in the evening to lower my cholesterol level. I still exercise a lot.
Impact on the family
8 I talked to my sons about genetics and their lifestyle risk factors and those of their children. As a result, one of my sons has given up smoking and the other one has improved his diet dramatically. They both exercise a lot, have very good diets, low in salt and saturated fats with lots of fruit and vegetables. They are both high achievers and ambitious and, as a result, are subjected to stress in their jobs. They are aware of the need to keep their cholesterol levels monitored and under control. Their children are given healthy diets, too.
9 For me, life goes on as before. For my family, the healthier lifestyle will prolong their lives.
10 I have mentioned the genetic risk of family heart problems to doctors in response to questioning or during a conversation. The information was only used as part of my diagnosis and was not followed up with any of my family. I have not had any discussions with nurses on the subject. It seems to me that people find out about genetic problems when it is too late to take any meaningful action. For example, why does the medical profession not have a more detailed discussion on genetics with parents when a baby is born or even earlier?
11 Collecting family histories is one useful way of determining possible genetic issues. I have found that my family members are very willing to talk about health issues in a constructive way. Recurring medical issues can be identified, and both genetic and environmental factors may be considered.
Final thoughts
12 From other activities that I now do, I am aware of two main issues affecting cardiac rehabilitation and lifestyle. One is to get patients to start cardiac rehabilitation and then to get them to continue with it. The other is persuading patients to continue to exercise and to follow a sensible diet after cardiac rehabilitation has ‘finished’.
13 I think that healthcare professionals have an important role to play in encouraging patients in these areas.
Educator touchpoints
Teaching moments
Paragraph 1 and 11 | What is a family history and why is it important?
Paragraph 4 | What genetic/genomic red flags and clues has Graham identified here as a possible reason for his condition?
Paragraph 4 | What routine health checks (for example, cholesterol checks) could have been carried out that may have identified issues?
Paragraph 5 and 6 | Even though the condition is genetic, what lifestyle changes can help reduce risk?
Discussion points
Paragraph 2 | Graham found some clues about the cause of his condition when talking to other patients in hospital. What could have been done differently to help him before this conversation happened?
Paragraph 5 | Where else could you signpost a patient with these questions?
Paragraph 10 | Why do you think the professional Graham interacted with didn’t pursue a genetic link earlier?
Paragraph 10 | What could be the some of the advantages and disadvantages of knowing this information at the point of birth for the patient and their family?
Paragraph 13 | Graham had to do his own investigations. What are the disadvantages of making a diagnostic leap without the support and guidance from healthcare professionals?
Further learning
FOUNDATION KNOWLEDGE
EXTENDED LEARNING
We explore how genomic information is passed from parent to child, and cell to cell
30 minutes
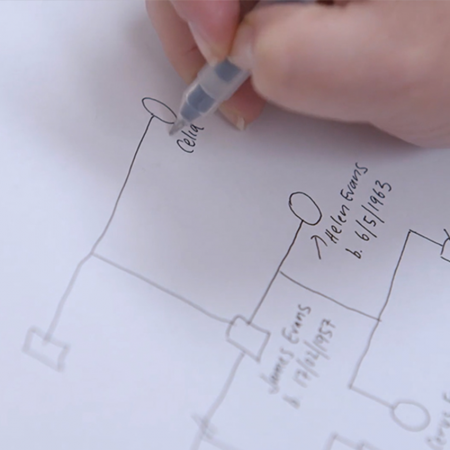
Learn about how a genetic family history can help to identify an inherited condition
30 minutes
Tips and tools for communicating with patients about genomics
30 minutes
Practical tips and tools to help you read, take and draw a genetic family history
15 minutes
Key facts about the condition, including its clinical features and genetic basis
5 minutes