The NHS’s new strategy for genomics: Five key takeaways
Image credit: North East and Yorkshire Genomic Medicine Service Alliance
We look at the new ‘Accelerating genomic medicine in the NHS’ report, an ambitious first in genomics strategy for the health service, and what it means for healthcare professionals
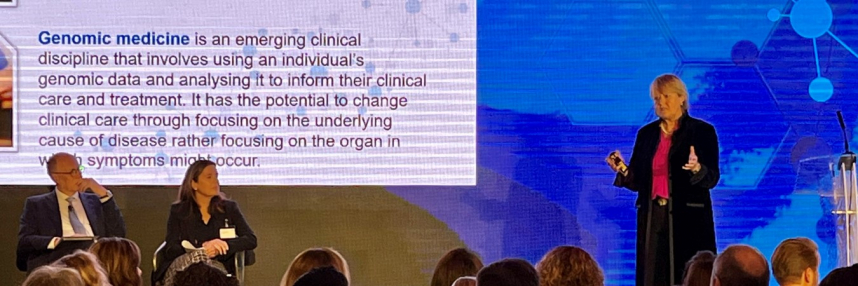
This month, NHS England released its first genomics strategy setting out how genomics and genomic technologies will be integrated into its healthcare services. The 64-page report was launched by NHS chief executive Amanda Pritchard and chief scientific officer for England Professor Dame Sue Hill.
‘Accelerating genomic medicine in the NHS’, details four priority areas to be delivered over the next five years:
- Embed genomics across the NHS, through a world leading innovative service model from primary and community care through to specialist and tertiary care.
- Deliver equitable genomic testing for improved outcomes in cancer, rare, inherited and common diseases and in enabling precision medicine and reducing adverse drug reactions.
- Enable genomics to be at the forefront of the data and digital revolution, ensuring genomic data can be interpreted and informed by other diagnostic and clinical data.
- Evolve the service through cutting-edge science, research and innovation to ensure that patients can benefit from rapid implementation of advances.
Here are five things we learned from the report:
1. WES out, WGS in, for children in intensive care
The NHS’s rapid whole exome sequencing (WES) service is being converted into a rapid whole genome sequencing (WGS) service for children in intensive care units (ICU).
WES – where only protein-coding genes are sequenced – started in October 2019 for paediatric ICUs. This genomic technology allowed 40% of those eligible to get or confirm a diagnosis, or have their care modified.
This year, the NHS will switch that to rapid WGS – where the majority of the patient’s genome is sequenced and relevant clinical findings are rapidly returned – so clinicians and specialist teams can “provide even greater diagnostic power” for children who would get the most benefit, such as those with cancer or rare genetic disease.
Additionally, WGS allows a newly discovered disease variant to be matched to existing and undiagnosed patients, letting children and their families complete the ‘diagnostic odyssey’.
In 2019’s Long Term Plan, the NHS aimed to be the first national healthcare system offering WGS in routine care. This expands upon that achievement, already made as part of the Genomic Medicine Service which offers genomic testing to eligible children and adults.
- Video (3 mins): Finding answers for patients through WGS
2. Pharmacogenomics’ growing role
Over the next three years, the NHS will look at which prescribing decisions can be informed by genomic testing. This will come from a review of internal and external knowledge.
NHS England spent £9.61 billion on prescription drugs in 2020, according to the NHS’s business services authority. Yet only about 30%-60% of prescribed drugs are effective, and adverse patient –drug reactions lead to 1-in-15 hospital admissions. This is costly for the NHS and negative for the patient.
Pharmacogenomics is important because it informs the clinician what drug, and at what dosage, their patient will best respond to.
An early step is putting pharmacogenomic information into electronic patient records and doing this in an expected way. NHS England will examine ongoing pilot projects to see what can be learned, before looking at a national roll-out of this standard.
Additionally, the NHS will work with organisations, like NICE and MHRA, to expand ‘companion diagnostic genomic testing’ – a test that uses the patient’s genome to help clinicians make prescribing decisions – that will help the NHS workforce access new medicines and technologies for patients.
Introducing pharmacogenomics into the clinic and bringing genomic data into the patient record benefits patients by making sure the right drug is prescribed to the right person, minimising adverse drug reactions.
- Further learning: What is pharmacogenomics?
- See also: Pharmacogenomics: three challenges to the NHS
3. Creating a new digital infrastructure
Integration in both human and computer systems is a major factor in the report, being mentioned in all four priority areas.
NHS England has a mixture of technologies that can prevent quick sharing of data. This is a named challenge for NHS providers to address.
A major goal is to develop common data standards, in what would be the first step in a fully connected digital infrastructure.
This genomics informatics implementation plan, to be delivered in 2023 by a newly established NHS Genomics Data and Digital Board, will also give clinicians the means to see where a sample is in its journey through the testing process.
Among clinicians, a standardised and common vocabulary has been encouraged.
Existing HPO (human phenotype ontology) terms are something of a dictionary. By using them, everyone involved in a complex patient case can communicate clearly and precisely on that patient’s care.
This ensures effective patient care among multi-disciplinary teams and accommodates new treatment options as they are developed.
4. Representing the patient voice
The patient voice is heard throughout the report through case studies that talk on how genomic technology and interventions have helped lead to a diagnosis.
An ethics advisory board will examine concerns about patient data protection and its use. Its purpose will be to understand how carers, patients and their families will be affected by the introduction of new technologies, such as RNA sequencing and detecting circulating tumour DNA in blood.
The board will be established within one to three years.
5. Genomics upskilling for all
“Not all healthcare professionals need to become genomic experts,” the report states, “but the workforce will need […] the skills and confidence to discern when testing may be relevant for their patients.”
Training and upskilling at all levels of the NHS will be done through royal societies, Health Education England’s Genomics Education Programme (GEP) and local genomic medicine services. It will include when and how to request genomic testing, and importantly how to have sensitive conversations with patients, families and carers about results.
The GEP’s own GeNotes (genomic notes for clinicians) was specifically picked out as an example resource. The upcoming Genomics Training Academy also was credited as a way to develop genomics skills in the existing and future NHS workforce.
Should you need a quick reference guide to the report’s commitments, you can find them in appendix two of the report.
–