Almost a miracle: gene-edited cells that can cure cancer
Since Layla Richards was cured of acute lymphoblastic leukaemia, attention has turned to the possibilities of genome engineering
Earlier this month, one-year old Layla Richards and her beaming family made front page news. Diagnosed with aggressive acute lymphoblastic leukaemia (ALL) at just three months of age, Layla went through chemotherapy and a failed bone marrow transplant in her first year, before doctors declared that there was nothing more that could be done. But, just months later, Layla is not only alive but cancer free and doing well. So just how did her medical team at Great Ormond Street Hospital reverse such a bleak (if accurate) prognosis?
Genius genome engineering
Researchers at Great Ormond Street (GOSH) and the UCL Institute of Child Health (ICH) have been working to develop treatments for some of the rarest and most intractable childhood diseases, including drug resistant cancers such as Layla’s ALL. The researchers are focusing on gene therapy, the underlying principle of which is that a patient’s own immune system T-cells can be genetically modified to recognise cancer cells and target them for destruction. However, some patients, like Layla, do not have enough T-cells for gene therapy to be effective, and so researchers have been working to develop a special type of alternative T-cells from healthy donors, using a form of targeted genome editing called TALENs.
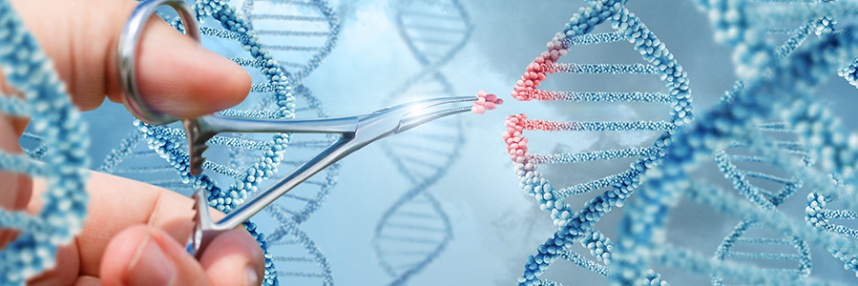
Genome editing is a revolutionary new technique that uses genetically engineered enzymes to introduce precise changes to DNA. The most commonly discussed approach is CRISPR, but TALENs (transcription activator-like effector nucleases) and ZFNs (zinc-finger nucleases) are alternatives that use a different type of enzyme as the ‘molecular scissors’ to cut DNA and direct insertion of a specific new section.
From mice to man
The researchers at GOSH and ICH used TALENs to edit the genome of healthy donor T-cells in two ways: masking the cell-surface molecules by which a patient’s immune system could recognise them as ‘foreign’; and adding other molecules that direct the T-cells to exclusively attack the patient’s cancer cells. The aim was to create a bank of special donor T-cells that could be customised to target different cancers in individual patients – the ultimate in designer gene therapy. Results in mice were promising; so promising, in fact, that special ethical approval was given for the approach to be used as a last-ditch attempt to save Layla, despite the fact that human safety trials had yet to take place.
To everyone’s delight, Layla’s treatment was a success. The donor T-cells successfully overpowered her leukaemia, after which she received another bone marrow transplant to repopulate her immune system. Whilst doctors have warned that it is still too early to tell whether it is a long-lasting cure, they have described the positive outcome of treatment as ‘staggering’. For Layla’s family, every day feels like a precious gift. And as the first successful therapeutic application of gene therapy for cancer in a human, Layla’s case is heralded as a landmark step towards personalised therapy – all thanks to human ingenuity unlocking the secrets of the genome.
–





 BBC/Minnow Films
BBC/Minnow Films