Circulating cell free DNA in pregnancy and cancer
Improved understanding of plasma DNA is opening up new possibilities for non-invasive testing and diagnosis
In the last few years, scientists have identified new possibilities for non-invasive testing by analysing cell free DNA circulating in the bloodstream. Non-invasive testing has revolutionised the field of prenatal diagnosis and is part of routine care; but a recent publication on the analysis of circulating tumour DNA (ctDNA) to predict relapse in breast cancer has highlighted the ways in which non-invasive testing could benefit cancer diagnosis and therapy too1, writes Fiona Macdonald.
A crucial discovery
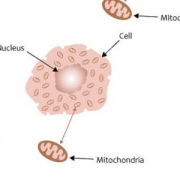
In 1997, cell free foetal DNA (cffDNA) was identified in the maternal circulation, and this has led to the development of non-invasive prenatal tests which pose no risk to pregnancy – in contrast to more established procedures such as amniocentesis. cffDNA is present from around seven weeks in pregnancy and rapidly cleared after delivery. Maternal plasma is therefore a mix of maternal and foetal DNA, with cffDNA constituting up to 10% of the total.
Initially diagnostic applications concentrated on detection of paternally inherited genetic sequences absent from the maternal genome. The first application focussed on the detection of Y-chromosome specific sequences, enabling foetal sex determination. This was valuable either for couples at risk of a foetus with an X-linked genetic disorder, or at risk of congenital adrenal hyperplasia (CAH), a condition for which a female foetus can be treated with dexamethasone to prevent virilisation.
Subsequently, testing was developed for monogenic disorders where the father was the affected parent, allowing detection of the paternal mutation in a quantitative assay similar to that used for Y-chromosome derived sequences. A similar approach has been used for de novo disorders such as achondroplasia, for which there is a small risk of recurrence in subsequent children. These tests are now well established within the NHS.
A bigger challenge
Detection of maternally derived gene alterations is much more challenging as the maternally derived portion of the foetal genome will add only a very small contribution over and above that of the mothers own DNA. Very accurate quantitation is required to detect such subtle changes in DNA levels. This kind of analysis requires sensitive technologies such as digital PCR, which uses a single molecule counting technique, or deep next generation sequencing (NGS).
Analysis follows either a targeted approach to look at one or a limited number of genetic areas of interest – for example, testing for autosomal recessive conditions such as beta-thalassemia – or a haplotyping approach, which is more cost effective. Haplotyping uses NGS and thousands of tiny DNA sequence variants spanning a gene of interest, alongside statistical analysis, to enable the identification of the foetal haplotype over and above the maternal haplotype. The feasibility of this method for diagnosis has been demonstrated in cases of both CAH and Duchenne muscular dystrophy. Both approaches have been developed to screen for chromosomal aneuploidies (abnormal chromosome number), responsible for conditions such as Down’s syndrome, in high risk pregnancies. Testing is now available commercially and is also offered through some regional genetics services.
Towards a ‘liquid biopsy’ for cancer monitoring
The realisation that dying tumour cells release DNA into the circulation (ctDNA) has opened up the possibility of non-invasive cancer diagnostics. This field has lagged behind that of prenatal diagnosis, as appropriate genomic positions for analysis were less well defined, but a large number of cancer genome sequencing studies have identified multiple genetic changes in tumours, expanding the whole area of biomarker research.
The identification of biomarkers such as the proteins EGFR in lung cancer, BRAF in melanoma, and KRAS in colorectal cancer (and their corresponding genes) is a technique used routinely in clinical practice to guide targeted chemotherapy. Expansion of the range of known markers in the majority of tumours has further advanced the field. Initial studies showed that identical genetic defects were seen in ctDNA and the primary tumours themselves; and as ctDNA is released from all areas of tumours, it is effectively a ‘liquid biopsy‘. Direct tumour biopsies remain the gold standard for cancer diagnosis, but these are invasive procedures with some risk to patients. They are also not always possible or practical, even where analysis of repeated samples could be of value, and ‘liquid biopsies’ provide an alternative.
DNA, predictive diagnosis and treatment
Analysis of ctDNA has a number of possible diagnostic applications. Changes in the level of ctDNA may indicate changes in the tumour burden. Identifiable ctDNA has been shown to correlate with the stage of cancer in a number of patients, while other tests have shown that the method can be used to identify whether a tumour is likely to respond to therapy. Analysis of serial plasma samples has also been used to identify mutations when cancer relapses after therapy.
The exciting potential for ctDNA was illustrated in a publication last month1. In a study of 55 early stage breast cancer patients who had received apparently curative treatments, analysis of ctDNA in serial plasma samples predicted relapse an average of 7.9 months ahead of clinical relapse in the majority of patients. In addition, massively parallel sequencing of ctDNA revealed the genetic basis for relapse. The implications of this for drug treatment ahead of relapse are unprecedented. More work is of course needed before this can be put into clinical practice. However, understanding of ctDNA is developing rapidly, and the availability of samples from the 100,000 Genomes Project will only accelerate progress.
Fiona Macdonald is a consultant clinical scientist based primarily in the West Midlands Regional Genetics Laboratory, and is a fellow of the Royal College of Pathologists. She is an author on more than 80 papers and has also written a variety of book chapters as well as co-authoring two books on the molecular basis of cancer.
References
- Garcia-Murillas et al (2015) Sci Trans Med, 7, 302ra133
–