Tetralogy of Fallot
Tetralogy of Fallot is a congenital heart anomaly that can be associated with underlying chromosomal conditions.
Overview
Tetralogy of Fallot is characterised by a combination of four specific heart anomalies. It can be detected antenatally or in the neonatal period by echocardiogram (cardiac ultrasound).
Clinical features
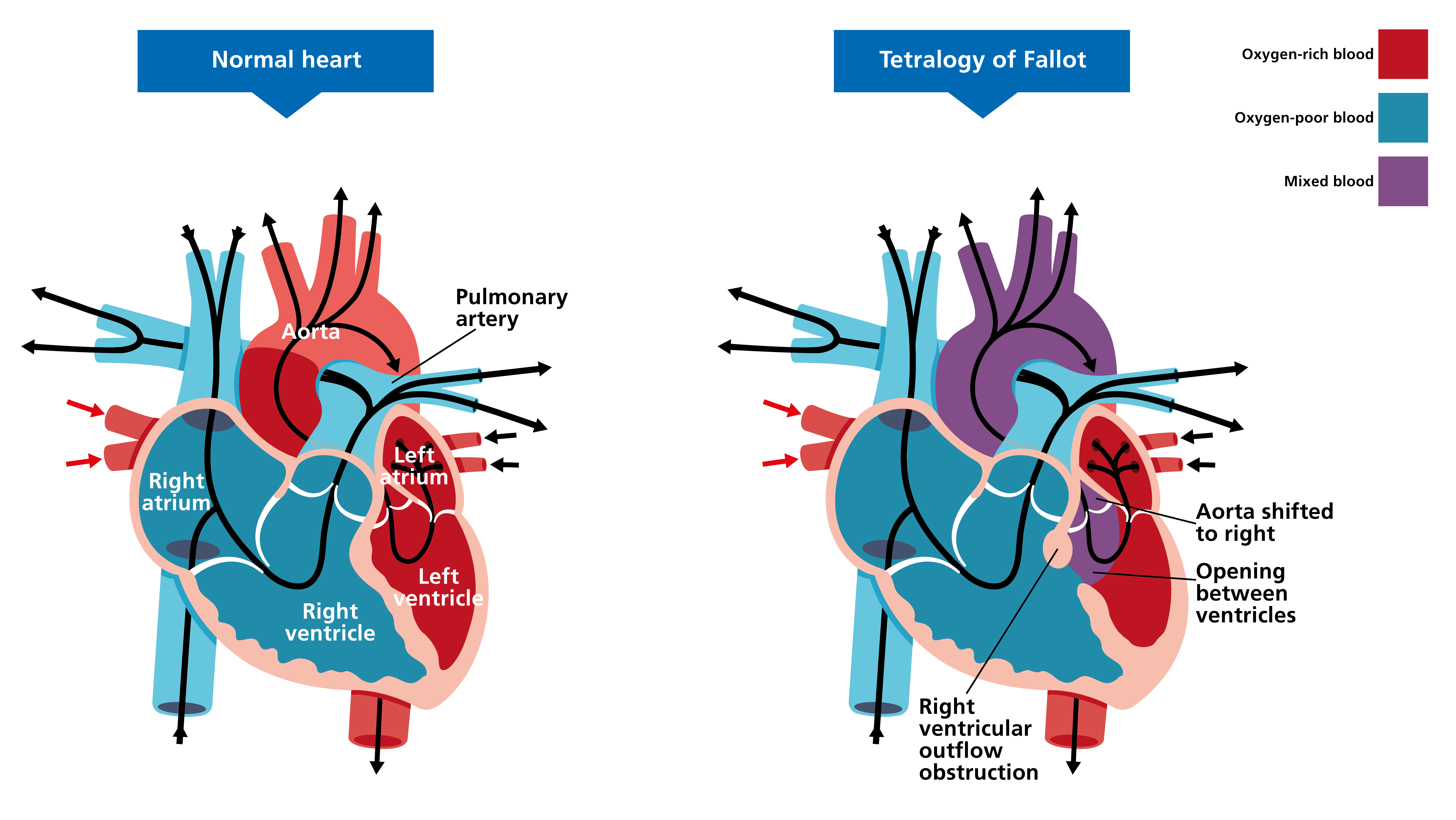
The clinical features of tetralogy of Fallot (ToF) are listed below. For a comparison with a normal heart, see figure 1.
- Overriding aorta: the aorta is positioned directly over a ventricular septal anomaly, instead of over the left ventricle.
- Pulmonary stenosis: a narrowing of the valve located between the right ventricle and the pulmonary arteries.
- Ventricular septal anomaly: a hole in the septum that separates the two ventricles of the heart.
- Right ventricular hypertrophy: an atypical enlargement in muscle mass of the right ventricle.
Figure 1: Clinical features of tetralogy of Fallot
Presenting features
Patients with ToF will present with some or all of the following symptoms:
- cyanosis;
- shortness of breath and rapid breathing, especially during feeding or exercise;
- floppy and/or pale appearance;
- poor weight gain;
- irritability;
- prolonged crying;
- heart murmur; and
- an atypical, rounded shape of the nail bed in the fingers and toes (clubbing).
Please note that symptoms vary, depending on the amount of blood flow.
Potential genetic causes
No genetic cause has been identified for the majority of ToF cases, though some patients may have additional anomalies and/or health issues that are part of a genetic syndrome.
Children with ToF, however, have an increased chance of having chromosomal conditions – see the following examples.
- 22q11.2 deletion syndrome: Also known as DiGeorge syndrome, this is caused by a microdeletion at chromosome position 22q11.2, which can be found with microarray, fluorescence in situ hybridisation (FISH) or targeted gene testing. Around 75% of patients with 22q11.2 deletion syndrome will have symptomatic congenital heart disease, of which ToF is one of the most common.
- Down syndrome: Caused by an extra copy of chromosome 21 (trisomy 21), found using QF-PCR testing. ToF occurs in around 6% of patients with Down syndrome and is the most common cyanotic heart anomaly to present in this patient group. Conversely, around 8% of patients with ToF have Down syndrome, although this is slightly higher in fetal series.
- Alagille syndrome: Caused by variants in either the JAG1 gene or the NOTCH2 gene, found with microarray, FISH or targeted gene testing. Around 90% of children with Alagille syndrome will have a heart anomaly, around 12% of which will be ToF.
Inheritance and genomic counselling
Isolated ToF has a multifactorial mode of inheritance in most cases, and recurrence risk rates of 2.5%–3% have been attributed to first-degree relatives of an affected child. In a subgroup of patients with a strong family history, the transmission of a monogenic trait has been suspected.
Management
Treatment comes in the form of major cardiac surgery, usually at around four to six months of age. Without the surgery, most children would sadly not live to adulthood. Dependent on the individual clinical picture, a shunt may be needed prior to the surgery. The majority of children will survive the surgery and have a good quality of life. In rare cases, further surgeries are required, and ongoing care from a cardiology team is recommended.
Resources
For clinicians
- Fetal Medicine Foundation: Second and third trimester: Tetralogy of Fallot
- Leeds Congenital Heart Unit: Tetralogy of Fallot
- NHS England: National Genomic Test Directory
For patients
- British Heart Foundation: Understanding your child’s heart: Tetralogy of Fallot
- International Society of Ultrasound in Obstetrics and Gynaecology: Tetralogy of Fallot