Key diagnostic terminology for skeletal dysplasia disorders
Familiarisation with specific terminology around skeletal dysplasias, used across several GeNotes resources, is important to appreciate the key differentials and identify the right genomic test.
Overview
Skeletal dysplasia disorders are classified according to Nosology and classification of genetic skeletal disorders, which is updated and published about every three years. Disorders are divided into broad categories based on clinical, radiographic or genetic unifiers (such as ‘conditions causing metaphyseal dysplasia’ or ‘mesomelic disorders’).
Types of limb shortening
The upper and lower limbs can be divided clinically and radiographically into three segments:
- Proximal, which corresponds to the humerus. If the segment is shortened, this is named rhizomelia (Greek origin: rhizo means ‘root’).
- Middle, corresponding to the radius and ulna. If shortened, this is named mesomelia (Greek origin: meso means ‘middle’).
- Distal, corresponding to the hand bones. If shortened, this is named acromelia (Greek origin: acro means ‘tip’).
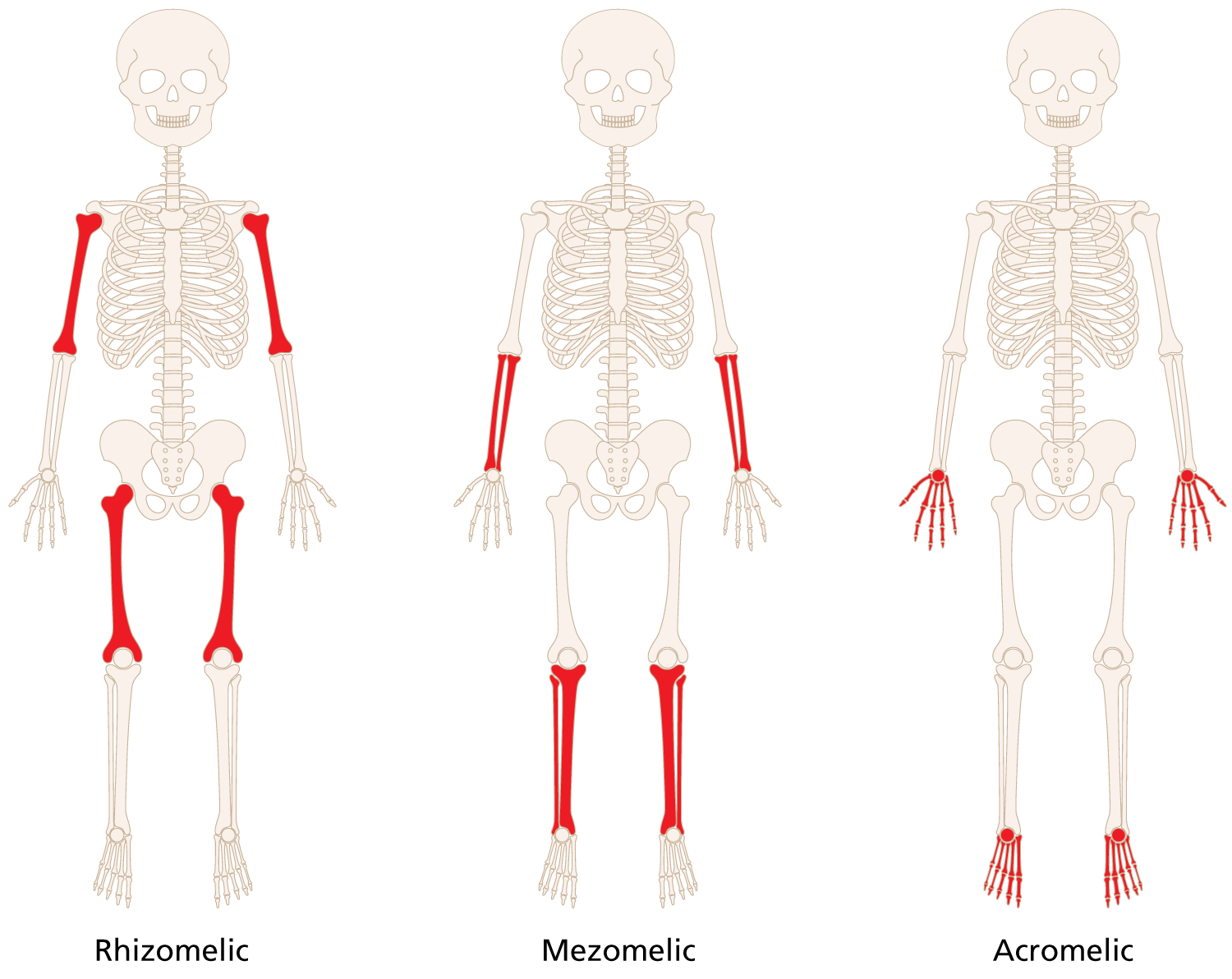 Figure 1: The three segments of limbs
Figure 1: The three segments of limbs
If all three segments are shortened, this is known as micromelia. If two adjacent sections are shortened, then the two names are combined; for example, mesomelia + acromelia = acromesomelia. By recognising such signs, the diagnosis is often narrowed to handful of differentials. For example, acromesomelia is specific to a few conditions under the acromesomelia dysplasia banner.
If mesomelia is present, the most common skeletal dysplasia to consider in the postnatal period is SHOX deficiency. See Presentation: Clinical suspicion of SHOX deficiency for information about genomic testing.
If rhizomelia is present, the most common skeletal dysplasias to consider in the postnatal period is achondroplasia and hypochondroplasia. See Presentation: Clinical suspicion of achondroplasia and Presentation: Clinical suspicion of hypochondroplasia for more information about genomic testing.
Key long bone changes
The long bones (and some short bones) are divided into three main sections:
- Diaphyses, which corresponds to the shaft. (Greek origin: dia means ‘passing through’.) If abnormally developed, this is called diaphyseal dysplasia.
- Metaphyses, which corresponds to the area ‘after’ the shaft that transitions in the epiphyses (neck of the long bone). It contains the growth plate. (Greek origin: meta means ‘after’ or ‘beyond’.) If abnormally developed, this is called metaphyseal dysplasia.
- Epiphyses, which corresponds to the end of the long bone (‘on top of’ the growth plate). (Greek origin: epi means ‘over’ or ‘on top of’.) If abnormally developed, this is called epiphyseal dysplasia.
Across all these terms, ‘physes’ means growth and refers to the growth plate.
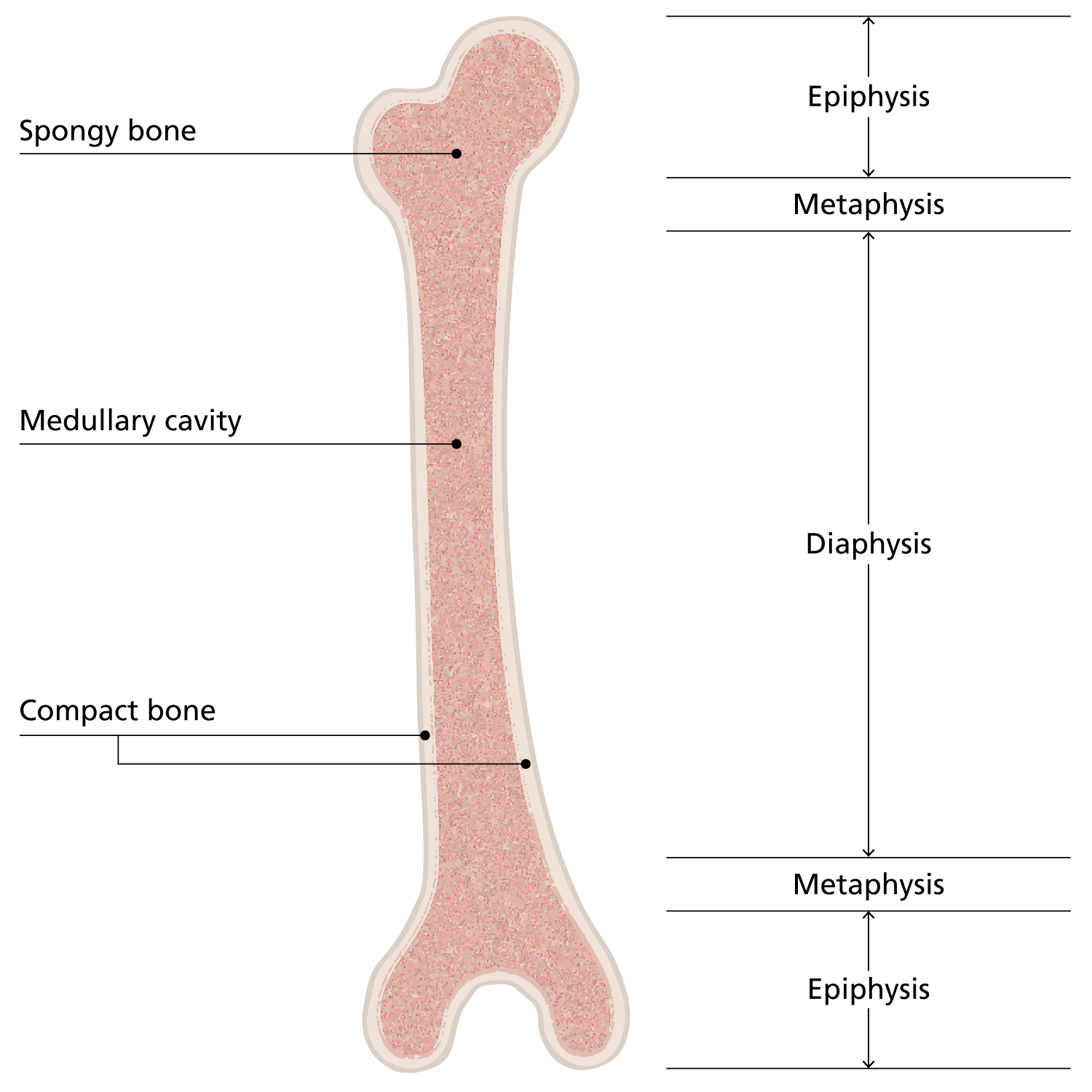
Figure 2: Structure of a long bone
Key spine changes
Changes in the development of spinal bones is an important part of classifying skeletal dysplasia conditions. Spinal changes (such as platyspondyly, meaning ‘flattened vertebrae’, or anisospondyly, meaning ‘abnormally increased size variability of vertebral bodies’) are referred to as spondylar dysplasia. The combination of spondylar dysplasia (S) with epiphyseal dysplasia (E) and/or metaphyseal dysplasia (M) lead to useful diagnostic umbrella groups, such as SED (spondylar epiphyseal dysplasia), SMD (spondylar metaphyseal dysplasia) and SEMD (spondylar epimetaphyseal dysplasia).
Further considerations
Knowing the above terms provides a good basis for describing and differentiating some of the key skeletal dysplasia disorders. Further terms and considerations that can help refine and direct your diagnosis include:
- the size of joints (such as enlarged / mega epiphyses);
- the shape of bones (such as slender or stubby);
- the density of the bones: osteopetrotic (dense) vs osteopenic (thin);
- presence of dislocations, fractures, bony lumps, stippling, striations, bowing, osteolysis, osteomyelitis and/or synostoses;
- presence of advanced or delayed ossification;
- a detailed description of any skull, chest, spine, hand, pelvic and patella bone changes; and
- involvement of other systems.
Familiarity with the key descriptors takes time to develop and can continue to be refined life-long. By considering the above clinico-radiological features, you will pick up more clues to help identify the most likely broad diagnostic categories. It will also enable you to input more relevant (human phenotype ontology) terms to aid your genomic testing. Remember, HPO terms are a key component in computer-driven analysis of genomic data in diagnostic searches.
Resources
For clinicians:
- Skeletal Dysplasia Group (teaching and research)
- Skeletal Dysplasia Management Consortium: Skeletal dysplasia best-practice guidelines
References:
- Unger S, Ferreira CR, Mortier GR and others. ‘Nosology of genetic skeletal disorders: 2023 revision’. American Journal of Medical Genetics Part A 2023: volume 191, issue 5, pages 1,164-1,209. DOI: 10.1002/ajmg.a.63132