Brugada syndrome
Brugada syndrome is an inherited arrhythmia condition that may manifest as syncope or sudden death (often during sleep) secondary to ventricular fibrillation in patients with a structurally normal heart.
Clinical features
- Clinical features of Brugada syndrome include palpitations, syncope and sudden death. The majority of affected individuals are asymptomatic.
- The first presentation of Brugada syndrome is commonly around 40 years of age. It is more prevalent in males of South East Asian ethnicity.
- The diagnostic electrocardiogram (ECG) finding is ‘coved’ ST segment elevation >0.2mV with T wave inversion in at least one right precordial lead (V1–V2) in the second, third or fourth intercostal spaces. This is known as the Brugada type 1 ECG pattern (see figure 1 below). Standard lead positions refer to V1–V2 in the fourth intercostal spaces; high lead positions refer to V1–V2 in the second or third intercostal spaces.
- The Brugada type 1 ECG pattern may be seen at rest (spontaneous type 1 Brugada ECG pattern) or with intercurrent fever or following administration of an intravenous sodium channel blocker such as ajmaline (inducible type 1 Brugada ECG pattern).
- Brugada syndrome is diagnosed in patients with a spontaneous type 1 pattern in the absence of other heart disease, regardless of symptoms. An induced type 1 pattern requires other clinical features, such as documented polymorphic ventricular tachycardia, ventricular fibrillation, arrhythmia syncope or relevant family history, to make the diagnosis.
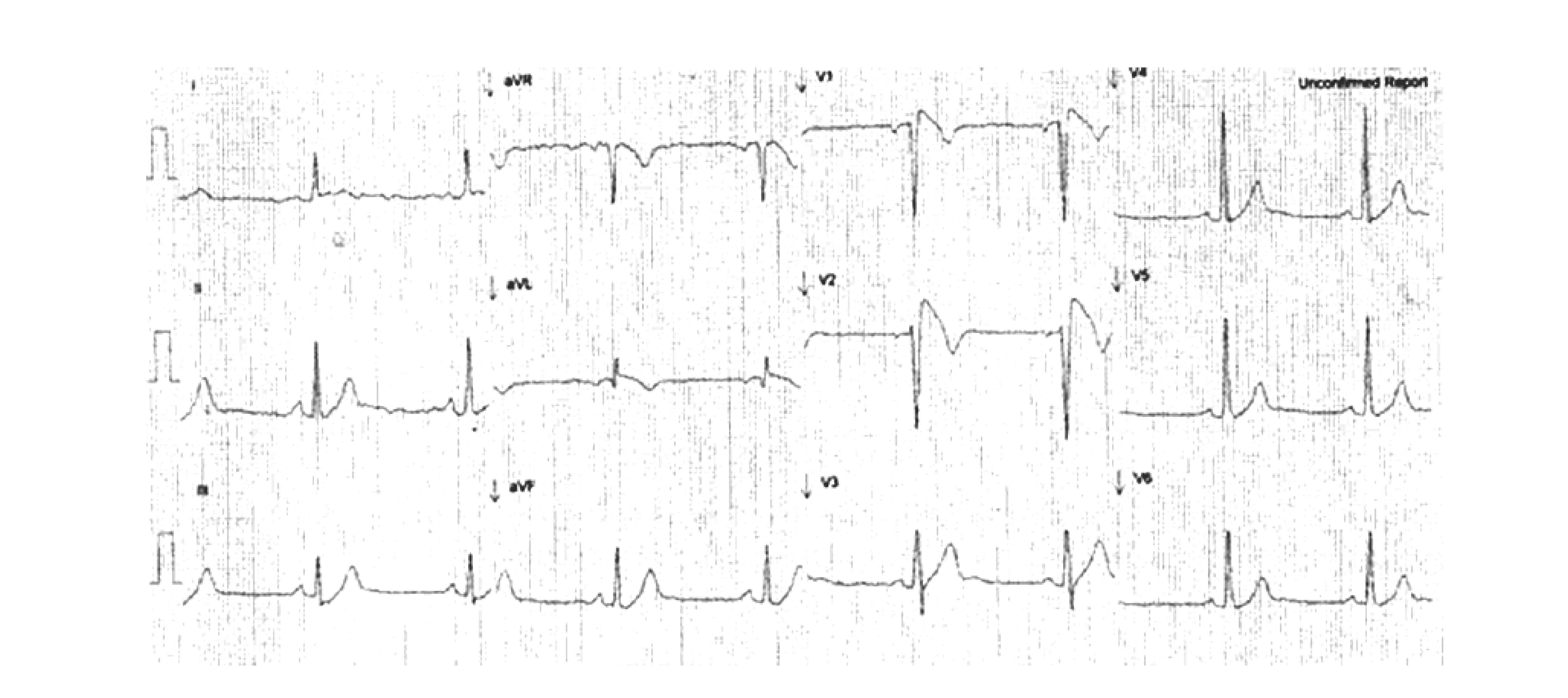
Figure 1: ECG demonstrating the type 1 Brugada ECG pattern in standard leads V1 and V2
Genetics
- The majority of patients with Brugada syndrome are not found to have a monogenic disease-causing variant. However, up to 20% of affected individuals have a pathogenic variant in the SCN5A gene, which encodes a subunit of the cardiac sodium channel responsible for regulating rapid sodium current in the heart.
- Pathogenic SCN5A variants are also associated with long QT syndrome type 3 and progressive cardiac conduction disease. Patients may describe some relatives with Brugada syndrome and others with different phenotypes; this would suggest the existence of overlap syndromes (that is, some family members experience different manifestations caused by the same genotype).
Inheritance and genomic counselling
- Most of the pathogenic variants associated with Brugada syndrome are inherited in an autosomal dominant pattern but can also arise de novo. There is variable penetrance, and although pathogenic variants are inherited equally by men and women, the phenotype appears to affect men more frequently.
- Recent research suggests that variants in genes other than SCN5A are also important in disease expression, following a polygenic mode of inheritance in some families. However, genomic testing via the National Genomic Test Directory does not currently support testing any genes other than SCN5A.
- All first-degree relatives of an individual with Brugada syndrome should be offered clinical screening in combination with genomic testing where appropriate. It is essential that this is undertaken in a specialist inherited cardiac conditions clinic due to the complexity of the inheritance pattern.
Management
- The mainstay of treatment in Brugada syndrome is careful lifestyle advice.
- Certain drugs may increase the likelihood of arrhythmia in the setting of Brugada syndrome. Patients should be directed to BrugadaDrugs.org for the list of drugs to avoid.
- Affected individuals should be given advice regarding prompt treatment of fever with antipyretics (such as paracetamol and ibuprofen) due to increased risk of arrhythmia.
- During a diarrhoea and vomiting illness, affected individuals should keep well hydrated using oral rehydration therapy (such as Dioralyte).
- Affected individuals should also be advised to avoid excessive alcohol consumption, cocaine and cannabis use and eating large meals before bed due to increased risk of arrhythmia.
- Implantable cardioverter-defibrillator (ICD) implantation is recommended in individuals who have survived cardiac arrest or have documented episodes of spontaneous ventricular arrhythmia.
- ICD implantation should be considered in individuals with a spontaneous type 1 Brugada ECG pattern and syncope.
- Asymptomatic affected individuals may undergo electrophysiology studies to assess whether there is inducible ventricular tachycardia or ventricular fibrillation.
- Affected individuals with recurrent ventricular arrhythmias may be treated using medication (such as quinidine) or with catheter ablation.
- Individuals with Brugada syndrome should be considered for genomic counselling (see the National Genomic Test Directory for eligibility criteria).
Resources
For clinicians
- National Organization for Rare Disorders: Brugada syndrome
- NHS England: National Genomic Test Directory
References:
- Zeppenfeld K, Tfelt-Hansen J, de Riva M and others. ‘2022 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Developed by the task force for the management of patients with ventricular arrhythmias and the prevention of sudden death of the European Society of Cardiology (ESC) endorsed by the Association for European Paediatric and Congenital Cardiology (AEPC)‘. European Heart Journal 2022: volume 43, issue 40, pages 3,997–4,126. DOI: 10.1093/eurheartj/ehac262
For patients
- British Heart Foundation: Brugada syndrome
- BrugadaDrugs.org
- Cardiac Risk in the Young
- NHS Health A to Z: Brugada syndrome