ACKR1/DARC-associated neutropenia
ACKR1/DARC-associated neutropenia is characterised by low blood neutrophil counts without increased infection risk. Its recognition is important when prescribing medications that require neutrophil count monitoring, such as clozapine and some types of chemotherapy.
Overview
ACKR1/DARC-associated neutropenia (ADAN) is characterised by low blood neutrophil counts without increased infection risk. The condition is also known as benign ethnic neutropenia (BEN) and Duffy-null associated neutrophil count (DANC).
ADAN is strongly associated with a homozygous variant in ACKR1 (c.-67T>C, rs2814778), which is known as the Duffy-null genotype (see ‘Genomics’ section). About 30% of people who have the Duffy-null genotype present with persistently low neutrophil counts, which is thought to be due to abnormal neutrophil migration from blood into tissues (figure 1).
People with ADAN are at risk of being excluded from treatments that require blood neutrophil counts to remain above a pre-defined threshold. Consequently, the recognition of ADAN has clinical importance.
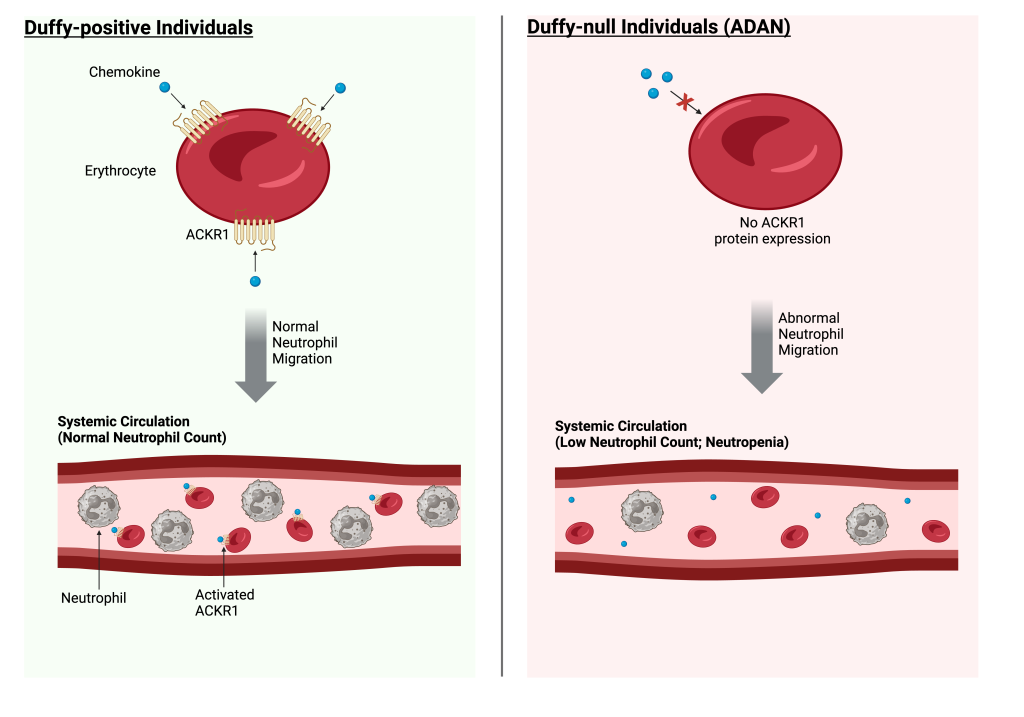
Figure 1: Neutrophil count in Duffy-positive and Duffy-null individuals. People who do not express ACKR1 protein on the surface of red blood cells, due to a homozygous variant in ACKR1 (Duffy-null), are associated with a lower-than-average blood neutrophil count (shown in the right-hand panel). This is due to altered chemokine signalling, which is mediated by the ACKR1 protein and leads to abnormal neutrophil migration. By contrast, people who express ACKR1 protein on the surface of red blood cells (Duffy-positive) do not have altered ACKR1-chemokine signalling, and therefore, have normal neutrophil migration between blood and tissues (shown in the left-hand panel).
(View larger size)
Clinical features
Indicators that a person may have ADAN include:
- persistently low absolute neutrophil counts observed over multiple blood measurements;
- no history of recurrent infections or other significant physical illness; and/or
- African or Middle Eastern ethnicity, although it should be noted that self-reported ethnicity can be an unreliable measure of genetic ancestry.
Genomics
ADAN is strongly associated with a homozygous variant in ACKR1 (c.-67T>C, rs2814778), which prevents transcription of ACKR1 in red blood cells. The homozygous variant is commonly known as the Duffy-null genotype, which refers to the Duffy blood group system.
The Duffy-null genotype is prevalent in people with African or Middle Eastern ancestry (~80% and ~25%, respectively), but is much less common in people with other ancestries, such as East Asian and European (<1%). This may have arisen due to selective pressures, as the Duffy-null genotype provides partial resistance to Plasmodium vivax malaria parasite infection.
Diagnosis
A diagnosis of ADAN requires confirmation by a haematologist. When ADAN is suspected (due to presence of relevant clinical features, see above), other potential causes of neutropenia must be ruled out to provide the diagnosis.
Additionally, genomic testing for the homozygous ACKR1 variant can help to confirm the diagnosis. Currently, ACKR1 genomic testing is not available via the National Genomic Test Directory; however, the test can be ordered by some haematology services. It is recommended to check whether the test can be ordered by your local haematology service.
If a person is confirmed to have the Duffy-null genotype (homozygous C/C at rs2814778), and they have isolated neutropenia without any significant physical illness, a diagnosis of ADAN can be made.
This guidance applies to adults only; suspected cases in children may require specialist consultation and possible further testing. Further guidance on the diagnostic pathway for ADAN can be found in these European guidelines.
Inheritance and genomic counselling
ADAN is inherited in an autosomal recessive pattern. This means that an individual must inherit two copies of the Duffy-null variant in ACKR1 (c.-67T>C, rs2814778), one from each parent, to be affected.
The prevalence of the Duffy-null variant in ACKR1 varies by genetic ancestry, and is estimated to be present in:
- 80% of people with African ancestry;
- 25% of people with Middle Eastern ancestry; and
- <1% of people with European or East Asian ancestry.
Management
When ADAN is confirmed, the managing clinician should discuss any relevant implications with the patient. This may require multidisciplinary input, such as from a haematologist, psychiatrist or oncologist, depending on whether the patient is receiving any treatment that may be adjusted following a diagnosis.
While ADAN itself requires no treatment, it is clinically relevant for individuals receiving treatments where neutrophil count monitoring is mandatory, such as clozapine and some types of chemotherapy. Where available, existing guidelines for the management of ADAN within these treatment groups should be followed to prevent unnecessary treatment interruption.
Resources
For clinicians
References:
- Atallah-Yunes SA, Ready A, Newburger PE. ‘Benign ethnic neutropenia‘. Blood Reviews 2019: volume 37. DOI: 10.1016/j.blre.2019.06.003
- Fioredda F, Skokowa J, Tamary H and others. ‘The European guidelines on diagnosis and management of neutropenia in adults and children: a consensus between the European Hematology Association and the EuNet-INNOCHRON COST Action‘. Hemasphere 2013: volume 7, issue 4. DOI: 10.1097/HS9.0000000000000872
- Howes RE, Patil AP, Piel FB and others. ‘The global distribution of the Duffy blood group‘. Nature Communications 2011: volume 2, article number 266. DOI: 10.1038/ncomms1265
- Hysong MR, Shuey MM, Huffman JE and others. ‘Characterization of the phenotypic consequences of the Duffy-null genotype‘. Blood Advances 2025: volume 9, issue 6, pages 1,452–1462. DOI: 10.1182/bloodadvances.2024014399
- Legge SE, Christensen RH, Petersen L and others. ‘The Duffy-null genotype and risk of infection‘. Human Molecular Genetics 2020: volume 29, issue 20, pages 3,349–3,349. DOI: 10.1093/hmg/ddaa208